Your breasts,
your future,
your choice.

Why get a mammogram?
Breasts may not be a go-to conversation topic, but talk leads to action and action is how we manage our breast health. So let's talk about them!
Get help scheduling a mammogram
Breast screening is covered by insurance
Commercial health insurers in Nevada are required to cover annual mammograms and other diagnostic imaging (like ultrasound for dense breasts) at no cost to the patient.
Here comes the uncomfortable (but necessary) part of the conversation.
In the United States, breast cancer is the most commonly diagnosed cancer in women. The good news is women have a way to fight back. Regular breast cancer screening — like mammograms and breast ultrasounds — is the best way to find breast cancer early when it is easier to treat. Here are three reasons you should get screened.

Breast screenings can detect breast cancer before you can feel a lump. Knowing what’s normal for you, whether it’s through monthly self-exams or just noticing any change, is important. So is the early detection that a screening provides. It’s not one or the other. For the best outcome, it’s both.
Breast cancer has a 99% cure rate when detected early. Annual mammograms can’t prevent you from getting breast cancer, but they can give you the best chance of surviving it.
Early detection reduces the risk of needing a mastectomy. When breast cancer is detected early, it is often possible to remove all cancerous cells with a procedure called a lumpectomy, rather than having to remove the entire breast.
Breast Cancer Affects
Black Women Differently

At any age, Black women are more likely to die from breast cancer.
Black women are 40% more likely to die from breast cancer than women of other races, and those younger than 50 are 50% more likely to die. Compared to other groups, Black women are at increased risk for more aggressive forms of breast cancer, such as triple-negative breast cancer and inflammatory breast cancer, which can be harder to treat. They are also more likely to be diagnosed with breast cancer at a younger age.
Black women are more likely to be affected by other risk factors.
Researchers found that Black women are more likely to have diabetes, heart disease, and obesity which are all risk factors for breast cancer. Additionally, certain products marketed to Black women may contain ingredients that could be linked to a higher risk of cancer, including hair relaxers and Brazilian blowout treatments. Whether the factors are individual, social, community, or environmental-related, Black women are at higher risk.
Black women are less likely to have access to health services.
Whether they are uninsured, underinsured, or simply do not have access to trusted providers and services in their community, Black women, more often than other groups, don’t get the screening, diagnosis, and treatment they need, when they need it. So when they get a breast cancer diagnosis, they often get it at a later stage when the cancer is more advanced.
Change the odds
Develop your own screening plan.
Because Black women are more likely to be diagnosed at younger ages and more advanced stages of the disease, it’s recommended they start screening early. While most women will begin screening at age 40, Black women and those with known risk factors may want to begin screening even earlier. Talk to your doctor about your risk and create a screening plan that makes sense for you.
A supplemental screening may be necessary
More aggressive types of breast cancer are often found with supplemental screenings, such as a breast ultrasound or a breast MRI. Women who have dense breast tissue may need a supplemental screening as well. Speak with your doctor about your risk factors, including race, and if you should get a supplemental screening.
Starting in January 2024, most insurers, including Medicaid, are required to cover all supplemental screenings at no cost.
Facts About Breast Cancer and Mammograms
Getting screened annually can help find breast cancer earlier when it’s easiest to treat and survive. Don’t let bad information, like these common myths, get between you and your health.
What to Expect When
Getting a Mammogram

What is a mammogram?
A mammogram is an X-ray of the breast. A mammogram offers a view of the breast that can show abnormalities before they are apparent to you or your doctor. Some facilities offer a 3D mammogram, which combines multiple breast X-rays to create a 3-dimensional picture of the breast.
How does it feel?
Some women find mammograms uncomfortable, some even find them painful, and for others, the procedure doesn't bother them at all. No matter what your experience, know that the technician is trained to provide gentle care, and any discomfort will last only a few seconds.
The procedure
On the day of your mammogram, don’t apply deodorant, antiperspirant, powders, lotions or perfumes on or under your breasts or underarms as these can cause white spots on the image
You’ll need to remove your top and bra, so wearing a skirt or pants may be easiest. The facility will give you a gown to wear. You’ll also want to remove necklaces and any large earrings and pull back longer hair.
Be sure to tell your radiology technologist if you have noticed any changes to your breasts, have implants, are breastfeeding or might be pregnant. Also, let them know if you have trouble standing or holding still for 30 seconds at a time.
To get a high-quality picture, your breast must be compressed for a short period. You'll stand in front of the machine and the technologist will position your breast on the machine. A plastic upper plate is then lowered to compress your breast while the technologist takes an X-ray.
Generally, two views of each breast are taken for a screening mammogram. For some women, such as those with larger breasts or implants, more images may be taken. The technologist will help you change position so your breast is compressed at a different angle before another X-ray is taken. The machine may move in an arc if you are getting a 3D mammogram.
The procedure typically takes less than 20 minutes, with actual breast compression lasting only 10–15 seconds for each image.
Adapted from American Cancer Society
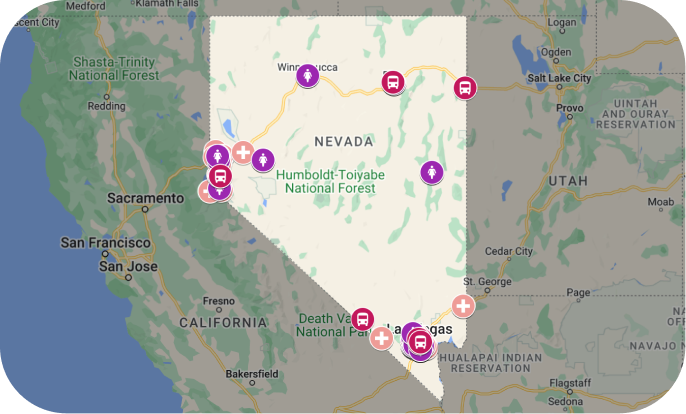
Free and Low-Cost Mammograms
No insurance? Underinsured? No problem. Several programs in Nevada provide free mammograms to those who are uninsured, cannot afford screening, and may not qualify for Medicare or Medicaid coverage.o problem. Several programs in Nevada provide free mammograms to those who are uninsured, cannot afford screening, and may not qualify for Medicare or Medicaid coverage.
Do you prefer one-on-one help getting a mammogram? Contact Nevada Cancer Coalition’s ThriveNV support team by calling 775-451-1670 ext 106.
Or complete this form.
Sources
- Journal of American Medical Association
- American Cancer Society
- Food & Drug Administration
- National Breast Cancer Foundation
- National Breast Cancer Coalition
- Susan G. Komen
- BreastCancer.org
- Breast Cancer Now
- Centers for Disease Control and Prevention
This material supported by Nevada Division of Public and Behavioral Health through Grants # NU58DP007102-02 and # 1NH750T000092-01-00 from the CDC.