Goal: Prevent cancer by reducing exposure to risk factors.

Reducing Nevada’s cancer burden begins with prioritizing prevention. The latest research finds that at least 40% of cancers cases and almost half of cancer deaths are caused by modifiable risk factors—those that can be prevented.xlv
The direct behavioral, physical, and environmental risks for cancer include smoking and tobacco use, excess body weight, alcohol consumption, physical inactivity, poor diet, exposure to ultraviolet radiation and radon, and infections such as human papillomavirus (HPV) and hepatitis C. Less direct, yet still important to acknowledge, are environmental factors such as exposure to secondhand smoke, occupational exposure to carcinogens, and cancer-causing contaminants in our air, water, and food.
| Risk Factor | Cancer Cases Attributable | Cancer Deaths Attributable | Top Types of Cancer |
|---|---|---|---|
| All risk factors combined | 40% | 44% | |
| Tobacco smoking and secondhand smoke | 23.1% | 29.2% | Lung, larynx, pharynx, oral cavity, esophagus, bladder, and kidney. |
| Excess body weight | 7.6% | 7.3% | Colorectal, breast, esophagus, gallbladder, kidney, liver, and pancreatic. |
| Alcohol consumption | 5.4% | 4.1% | Liver, breast, mouth, throat, esophagus, and colon. |
| Ultraviolet radiation | 4.6% | 1.3% | Skin. |
| Poor diet | 4.2% | 4.3% | Colorectal, stomach, breast, and pancreatic. |
| Infections | 3.4% | 3.5% | Liver, cervix, stomach, oropharyngeal, penile, anal. |
| Physical inactivity | 3.1% | 2.5% | Colorectal, endometrial, lung, and breast. |
HPV Objectives and Indicators
Reversing the Trend for HPV Vaccination
HPV vaccination rates in Nevada improved steadily until the COVID-19 pandemic, which caused progress to stall and decline slightly, especially among adolescents and young adults in rural areas. Recent years have not seen a full recovery to pre-pandemic coverage levels, and disparities by geography and gender persist. Nearly half of Nevada adolescents ages 13-17 haven’t received a first dose of HPV vaccine, and of those who did receive a first dose, nearly one-third did not receive a second. Policy changes have expanded adult vaccination, but adolescent coverage—critical for cancer prevention—remains below optimal levels.
Objective: Increase HPV vaccine series initiation and completion among Nevada youth.
Strategies:
- Establish standard recommendation language for HPV vaccination regarding age of initiation.
- Support efforts and campaigns to increase HPV vaccination among Nevada youth.
- Ensure language accessibility and equity in all HPV vaccination material and campaigns.
- Recruit experts and champions to participate in HPV vaccination campaigns, support educational opportunities, and participate in other collaborative efforts.
- Educate clinicians on evidence-based strategies to increase initiation and completion of the HPV vaccination series.
- Support ongoing policy and advocacy efforts to increase HPV vaccination rates.
Indicators
Percentage of 9-year-olds who received at least one dose of HPV vaccine.
Baseline: 9.1%
Target: 9.6%
Percentage of youth age 17 or younger who have completed the HPV vaccination series.
Baseline: 38.7%
Target: 66.1%
Source: Nevada State Immunization Program
Physical Activity and Nutrition Objectives and Indicators
Physical Activity and Nutrition to Reduce Cancer Risk
While no single food or type of physical activity can prevent cancer, evidence strongly demonstrates the cumulative effect of healthy diet and regular physical activity on reducing cancer risk. Years of research have found diets high in fiber that prioritize plant-based foods, whole grains, lean meats and fish, and limit processed and red meats, refined sugars, and alcohol are linked to reduced overall cancer risk. Multiple studies have also shown that physical activity—from light-intensity activities such as household chores or walking to moderate to vigorous exercise—can reduce risk for multiple cancers, regardless of body weight or other health conditions. xlviii, xlix, l
There are many ways physical activity and diet help to prevent cancer:
- Reducing DNA damage, inflammation, and oxidative stress on the body that can contribute to cancer development.
- Lowering levels of hormones like estrogen and insulin that can reduce development or progression of cancer.
- Supporting immune function that can eliminate abnormal cells and inhibit tumor growth.
- Helping to maintain a healthy weight. Being overweight or obese is a factor in up to 20% of cancer deaths.
Both a healthy diet and physical activity can play a role in maintaining a normal body weight and avoiding obesity and its related health complications. However, innovations in the treatment of obesity with GLP-1 receptor agonists, such as semaglutide, should also be recognized as tools to reduce the risk of obesity-associated cancers and address some biological mechanisms that increase cancer risk, such as inflammation and poor metabolic health.li Researchers have found GLP-1 RAs can significantly reduce the risk of at least 10 obesity-related cancers including colorectal, kidney, liver, ovarian, and pancreatic cancers.lii
There are also factors beyond an individual’s personal behaviors that may influence one’s ability to engage in physical activity and consume a nutritious diet. Broader community approaches to address the root causes of inactivity and poor nutrition require engagement with community leaders to foster active transportation and access to parks and outdoor recreation, reduce air pollution and heat islands, increase tree canopy, and develop food systems that improve access to grocery stores, farmers markets, and community gardens.
Alcohol and Cancer
Alcohol is a known carcinogen, increasing the risk for at least seven types of cancer including mouth, throat, larynx, esophagus, breast, liver, and colorectal. Researchers first established the link between alcohol and cancer in the 1980s, and the body of research showing the causal link between alcohol and cancer has only grown since then. Despite this, fewer than half of U.S. adults are aware that alcohol can increase cancer risk, and in some instances, they mistakenly believe it can reduce cancer risk. An estimated six in 10 U.S. adults say they consume alcohol, and in Nevada 17% of adults report heavy or binge drinking.liii, liv
Heavy drinking is defined as 14 drinks per week for men or 7 drinks per week for women. Binge drinking focuses on a large quantity of drinks on a single occasion, measured as five or more drinks for men or four or more drinks for women. A standard drink of alcohol is generally 12 ounces of beer, five ounces of wine, or 1.5 ounces of distilled spirits.
Alcohol increases cancer risk by:
- Breaking down into substances that damage DNA and increase oxidative stress and inflammation in the body.
- Altering hormone levels, including estrogen, which can increase breast cancer risk.
- Dissolving carcinogens from other sources, especially particles from tobacco smoke, that are more easily absorbed into the body.
Alcohol and tobacco use together increases cancer risk even more, and interventions that address both can be especially effective at reducing Nevada’s cancer burden. Lessons learned from tobacco control can be applied to reducing alcohol use, and best practices, such as reducing stigma and de-normalizing consumption, may be especially effective.
Objective: Improve the fitness and nutrition of children, adolescents, and adults in Nevada.
Strategies:
- Educate the public on obesity and alcohol consumption as risks for cancer.
- Expand access to free, safe, and appealing water sources in schools and eliminate access to sugar-sweetened drinks.
- Promote education and resources for lactating parents to increase chest/breastfeeding rates to reduce childhood obesity.
- Support and implement evidence-based strategies that promote healthy behaviors in places where people live, learn, work, play, and worship.
- Support efforts to strengthen evidence-based school wellness policies to improve nutrition and physical activity, including universal school lunches.
- Support policies and programs for active living, including built environment and community design.
- Support policies and programs that increase access to nutritious food and reduce food insecurity.
- Advocate for sustainable funding to support obesity surveillance, prevention, and treatment programs.
- Support efforts to expand insurance coverage for evidence-based healthy weight management programs and anti-obesity medications.
Indicators:
Increase elementary, middle, and high school students who have a healthy weight based on BMI.
Baseline: 71.1%/65.6%/62.8%
Target: 75%/69%/66%
Source: School Screening in Nevada dashboard.
Increase adults who are physically active
Baseline: 31%
Target: 35%
U.S.: 30.4%
Source: BRFSS
Decrease adults who are heavy drinkers
Baseline: 6.7%
Target: 5.5%
U.S.: 6.1%
Source: BRFSS
Tobacco Objectives and Indicators
A Look at Tobacco Disparities
The tobacco industry has targeted some communities more than others for decades through advertising and promotions, often focusing on individuals who are people of color or members of the LGBTQ+ community. Menthol products have been heavily marketed to Black and LGBTQ+ people and are known to be more appealing to new or younger tobacco users and harder to quit. Data from the 2023 Adult Tobacco Survey shows that Black, Pacific Islander, American Indian and Hispanic Nevadans smoke tobacco at higher rates, with menthol tobacco smoked by more than half of Black tobacco users. People who are not heterosexual use tobacco at more than twice the rate of heterosexual people in Nevada, are seven times as likely to use smokeless tobacco, and are more than four times as likely to use e-cigarettes, however they are less likely to have been advised to quit tobacco at their last doctor’s visit.lv
The CDC notes that increased stress and discrimination faced by many people in communities of color or who are LGBTQ+ makes individuals in these groups more likely to smoke or use tobacco and e-cigarettes.lvi
E-Cigarettes: Should We Worry?
While decades of research have firmly established the link between smoking and tobacco use to cancer, research on the cancer risks caused by vaping and e-cigarettes remains preliminary but increasingly concerning. The aerosols inhaled when vaping contain harmful chemicals that are known carcinogens which can damage DNA and increase inflammation—both key factors in cancer development. Dual users of cigarettes and e-cigarettes have a significantly higher risk of lung cancer than smoking alone. lvii,lviii
Objective: Decrease the percentage of youth (grades 9-12) who have reported smoking cigarettes or using electronic vapor products in the past 30 days.
Strategies:
- Decrease youth and young adult exposure to commercial tobacco, vapor, and related products.
- Expand and promote awareness of cessation resources designed for youth and young adults.
- Promote stronger tobacco retail licensure requirements to increase compliance with laws and policies restricting minors' access to tobacco and electronic smoking devices.
- Advance policy to further regulate and curtail the sale and use of tobacco, vapor, and related products to reduce youth access.
Objective: Reduce the percentage of adults who smoke and increase the percentage of adults who are former electronic smoking device users.
Strategies:
- Increase access and referrals to tobacco cessation services and resources in health care settings and via educational campaigns.
- Educate stakeholders and decision-makers about evidence-based policies and programs to increase cessation.
Objective: Improve the Nevada Clean Indoor Air Act (NCIAA) that prohibits smoking in public places and worksites by decreasing the number of exemptions.
Strategies:
- Collect, evaluate, and share data on secondhand smoke and emissions from electronic smoking devices.
- Support modernization of the NCIAA and related statutes.
- Support policies for smoke-free and vape-free workplaces by continuing to educate lawmakers, business owners, and the general public on the benefits of smoke-free workplaces.
Indicators:
Youth Who Smoked Tobacco, past 30 days
Baseline: 2.9%
Target: 2.5%
U.S.: 3.5%
Source: Nevada YRBS
Youth Who Used Vapor/E-Cigarette Products, past 30 days
Baseline: 15.1%
Target: 14.5%
U.S.: 16.8%
Source: Nevada YRBS
Adults Who Smoke Tobacco
Baseline: 14.2%
Target: 13.5%
U.S.: 12.1%
Source: BRFSS
Former Electronic Vapor Users
Baseline: 22.1%
Target: 23.9%
U.S.: 19.4%
Source: BRFSS
NCIAA Exemptions Eliminated
Baseline: 0
Target: 2
Radon Objective and Indicators
What is Radon?
Radon is a naturally occurring, colorless, odorless radioactive gas that can cause lung cancer when it becomes trapped indoors after entering a building through tiny cracks in the foundation. Testing homes, offices, schools, and other workplaces for the presence of radon can help to identify elevated levels of the gas. Once identified, systems can be put in place to mitigate radon exposure, such as by venting the gas outside.
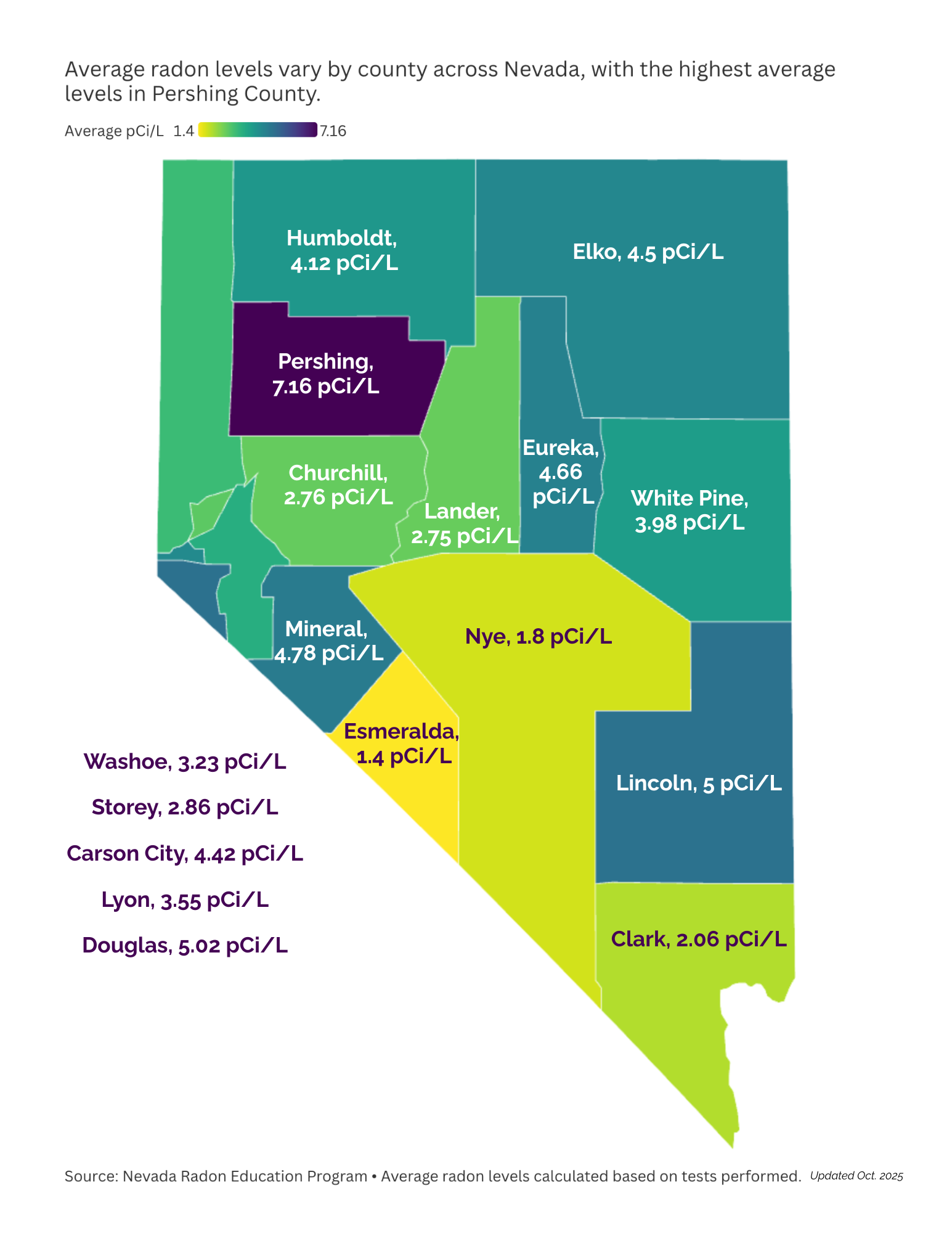
Objective: Decrease exposure to elevated levels of radon.
Strategies:
- Educate healthcare professionals and partners on radon risks, integrating testing questions into patient questionnaires and clinic practices.
- Distribute awareness materials in healthcare facilities.
- Support partner promotional campaigns on radon education, testing, and mitigation.
- Integrate radon education into broader public health initiatives, such as tobacco cessation efforts and the Nevada Tobacco Quitline.
- Train individuals in every county on radon testing and provide test kits for local distribution.
- Expand radon testing access in underserved and rural communities through targeted programs.
- Introduce a public library lending program for radon test kits.
- Promote certification programs to expand the radon mitigation workforce, especially in underserved areas.
- Collect, analyze, and publish data on radon testing, mitigation, and radon-resistant construction adoption.
- Track and set targets for radon testing in real estate transactions to improve compliance and awareness.
- Support policies requiring radon-resistant construction in new homes and for licensing of radon mitigation professionals.
Indicators
Valid radon home tests completed
Baseline: 46,100
Target: 61,000
Existing homes mitigated for radon
Baseline: 2,814
Target: 3,800
New homes built radon resistant
Baseline: 719
Target: 900
Source: Nevada Radon Education Program
Sun Safety Objective and Indicator
Sun Smart for Skin
Given Nevada's average elevation of 5,500 feet, around 250 sunny days per year and our love of the outdoor lifestyle, Nevadans are at higher risk for skin cancer. Historically, the rate of melanoma diagnoses has shown an upward trend, yet so have sun smart efforts in many communities. Skin cancer takes a number of years to develop, so progress made now to improve sun safety will not yield results for a number of years. Expanded partnerships with dermatologists and medical schools at both University of Nevada, Reno and University of Nevada, Las Vegas, have increased our state’s ability to engage with Nevadans and build a community of sun safety champions.
Objective: Reduce the incidence of skin cancer.
Strategies:
- Promote sun safety and skin cancer prevention and early detection education through Sun Smart Schools and Sun Smart Nevada programs.
- Collaborate with event coordinators to integrate shade and sunscreen access into community events.
- Partner with communities to foster sun-safe environments and education.
- Advocate for sun-safe built environments especially in preK-12 schools.
- Work with businesses to promote sun and heat safety for outdoor workers and others with occupational risk of UV radiation.
- Educate the public on indoor tanning restrictions for minors and ensure tanning establishments comply with state law.
Indicator
Incidence of melanoma
Baseline: 23.5 per 100,000
Target: 22.3 per 100,000
References
xlv Nierengarten, M. B. "High percentage of cancers potentially preventable." Cancer, vol. 130, 2024, pp. 3620-3620, https://doi.org/10.1002/cncr.35577.
xlvi Islami, F., E. C. Marlow, B. Thomson, et al. "Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States, 2019." CA: A Cancer Journal for Clinicians, vol. 74, no. 5, 2024, pp. 405-432, doi:10.3322/caac.21858.
xlviii Torres, Á., F. Quintanilla, E. Barnafi, C. Sánchez, F. Acevedo, B. Walbaum, T. Merino. "Dietary Interventions for Cancer Prevention: An Update to ACS International Guidelines." Nutrients, vol. 16, no. 17, 2024, p. 2897, doi:10.3390/nu16172897.
xlix Shreves, A. H., S. R. Small, R. Walmsley, et al. "Amount and intensity of daily total physical activity, step count and risk of incident cancer in the UK Biobank." British Journal of Sports Medicine, 26 Mar. 2025, doi:10.1136/bjsports-2024-109360.
l Simon, Stacy. "How Exercise Can Lower Cancer Risk." Cancer.org, 2020, https://www.cancer.org/cancer/latest-news/how-exercise-can-lower-cancer-risk.html.
li Wolff Sagy, Yael, et al. "Glucagon-like peptide-1 receptor agonists compared with bariatric metabolic surgery and the risk of obesity-related cancer: an observational, retrospective cohort study." eClinicalMedicine, vol. 0, no. 0, 2025, p. 103213.
lii Wang, L., R. Xu, D. C. Kaelber, N. A. Berger. "Glucagon-Like Peptide 1 Receptor Agonists and 13 Obesity-Associated Cancers in Patients With Type 2 Diabetes." JAMA Network Open, vol. 7, no. 7, 2024, e2421305, doi:10.1001/jamanetworkopen.2024.21305.
liii U.S. Department of Health and Human Services. "Alcohol and Cancer." https://www.hhs.gov/surgeongeneral/reports-and-publications/alcohol-cancer/index.html.
lv Nevada Institute for Children’s Research & Policy. Nevada Statewide Adult Tobacco Survey 2023. Apr. 2024, https://gethealthyclarkcounty.org/wp-content/uploads/2024/09/2023-Nevada-Adult-Tobacco-Survey.pdf.
lvi Centers for Disease Control and Prevention. "Unfair and Unjust Practices Harm LGBTQ+ People and Drive Health Disparities. Smoking & Tobacco Use." 26 Jan. 2023, https://www.cdc.gov/tobacco/health-equity/lgbtq/unfair-and-unjust.html.
lvii Sahu, R., K. Shah, R. Malviya, D. Paliwal, S. Sagar, S. Singh, B. G. Prajapati, S. Bhattacharya. "E-Cigarettes and Associated Health Risks: An Update on Cancer Potential." Advances in Respiratory Medicine, vol. 91, no. 6, 2023, pp. 516-531, doi:10.3390/arm91060038.
lviii American Cancer Society. "Smoking and Vaping Together Increases Lung Cancer Risk More Than Smoking Alone." https://www.cancer.org/cancer/latest-news/smoking-and-vaping-together-increases-lung-cancer-risk-more-than-smoking-alone.html.